Indicators
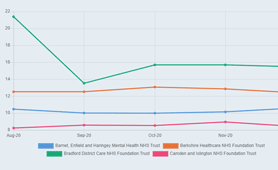
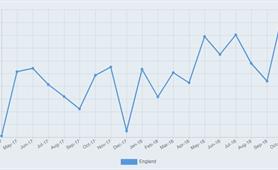
These indicators help you check on how well the system is performing in terms of access to care.
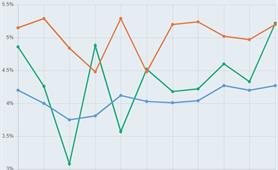
These indicators allow you to check how well the system is performing in terms of the way care is provided.
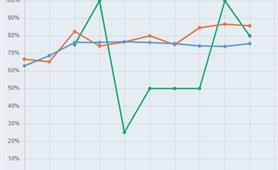
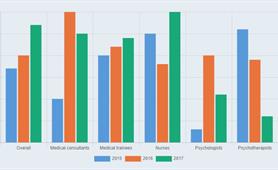
These indicators help you check how the system is performing in terms of those delivering care: are there enough people, what is their morale like, how do they view the quality of care provided?
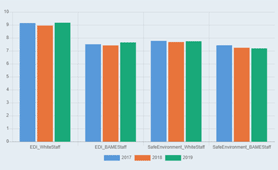
This category helps you check how well led organisations are, based on ratings and perceptions of those working in the organisations.
Our finance indicators relate to the data about how much is being invested across a range of areas in mental health.
Sorry there is no current indicator









.tmb-thumb.png?Culture=en&sfvrsn=77a1fad1_2)